
You may have heard of occupational therapy (OT) and physical therapy (PT) and not really understood the difference. The difference between these two types of therapy is that occupational therapy focuses on the body’s ability to perform certain tasks, while physical therapy focuses on improving a person’s body movement. OT is specifically aimed at helping people with common daily functions. Most OT patients are challenged by a cognitive issue or a physical and/or sensory disability that affects their physical abilities.
There are over 20 different types of occupational therapy. For the purposes of this page we will be addressing a general description of what some of the common occupational therapy types and techniques entail. This should not be considered to be an all-inclusive list.
Occupational Therapy Interventions include
- Occupations and activities – These types of interventions refer to activities that can be done every day or have a therapeutic purpose. Bathing, dressing and feeding are all examples of interventions that fall within this category.
- Preparatory methods and tasks – These types of interventions involve the use of adaptive devices and techniques to help prepare a patient for a specific activity or help them reach their ultimate goal. Take for example a patient recovering from a stroke who’s lost mobility and strength in their hands. They want to be able to feed themselves. An OT may ask the patient to use therapy putty for exercises that will help them regain strength and movement in their hands, rather than having them attempt to feed themselves straight away. The use of therapy putty in this case is a preparatory intervention.
- Education and training – Education and training can be beneficial to both patients and their caregivers. Through education and training both parties receive useful information to guide through the treatment process, and in some cases, after the process. Through this type of intervention, a parent or caregiver might learn how to use and support their loved one in the use of an adaptive device.
- Advocacy – Advocacy interventions range from cheering on a patient during treatment to teaching them how to advocate for their own needs. An OT may also find themselves advocating for their patient population by serving on the board of an organization seeking to effect policy changes within the field.
- Group interventions – Occupational therapists identify opportunities for patients to be a part of a collaborative environment that will be beneficial to their treatment process, recovery and overall wellbeing.
Types of Occupational Therapy Specialties

Assistive Technology (AT): Assistive technology is any item, piece of equipment, software program, or product system that is used to increase, maintain, or improve the functional capabilities of persons with disabilities. Assistive technology helps people who have difficulty speaking, typing, writing, remembering, pointing, seeing, hearing, learning, walking, and many other things. Different disabilities require different assistive technologies. AT products can be made by hand, purchased off the shelf, or adapted from an existing product.
Assistive technology (AT) has two parts: devices (the actual tools people use) and services (the support to choose and use the tools).
Services can include:
- Evaluation of needs (initial and follow-up evaluations)
- Purchasing, leasing, loaning, or otherwise providing for acquiring assistive technology devices
- Selecting, designing, fitting, cusomizing, adapting, applying, retaining, repairing, or replacing assistive technology devices
- Coordinating interventions, services, therapies (such as is done in rehab programs or schools)
- Training and technical assistance for employers, professionals, providers, caregivers, etc
Devices can include:
- AT can be basic: markers, highlighters, white boards, calendars, timers, etc
- AT can be physical products: wheelchairs, glasses, prosthetic limbs, braces, white canes, walkers, canes, and hearing aids.
- AT can be low-tech: communication boards made of cardboard or fuzzy felt.
- AT can be high-tech: special-purpose computers, speech recognition or time management software, screen reading software, captioning, or mobility devices.
- AT can be hardware: prosthetics, mounting systems, and positioning devices.
- AT can be computer hardware: special switches, keyboards, and pointing devices.
- AT can be computer software: screen readers and communication programs.
- AT can be inclusive or specialized learning materials and curriculum aids.
- AT can be specialized curricular software.
- AT can be much more—electronic devices, wheelchairs, walkers, braces, educational software, power lifts, pencil holders, eye-gaze and head trackers, and much more.
AT devices that may be utilized in school (elementary, middle, high, and college) include:
- Academic and learning aids: calculators, spell checkers, word processors, computer software, adapted timers and watches, adapted knobs, picture-based instructions for how to do a job, adapted books, switch-operated toys, etc
- Daily Living Aids: devices for eating, bathing, cooking, dressing, toileting, etc.
- Assistive visual devices: magnifiers, talking calculators, Braille writers, screen reading software, Braille note-taking devices, etc.
- Assistive listening devices: amplification devices, close captioning systems, environmental alert systems, etc.
- Augmentative communication: electronic and non-electronic tools that help students communicate
- Computer access: modified keyboards, switches, special software, alternative access aids
- Environmental control: switches, adapted appliances, environmental control units
- Mobility devices: wheelchairs, walkers, canes, scooters, corner chairs, wedges, prone standers, wedge seats, adapted/alternative chairs, and other devices that help the person move around
Training required to be an Assistive Technology professional:
- A variety of educational backgrounds are accepted, ranging from high school diploma to Master’s degree or higher
- Total hours of assistive tech-related training will depend on the degree received (10, 20, or 30 hours)
- Half of training hours need to be met at IACET or University approved continuing education units; the other half may be fulfilled by other Continuing Education Credits or documented contact hours
- Training hours must be completed in same time frame as your work experience

Autism: Occupational therapists may work with patients who have autism and need help with developing their motor skills, learning strategies, social skills and self-care. They also help patients with their independence while doing these everyday activities:
- Dressing
- Grooming
- Personal care routines
- Using utensils
- Play activities
People with autism have varying capabilities so the responsibilities of the OT differ from patient to patient. You can earn the certified autism specialist credential from the International Board of Credentialing and Continuing Education Standards (IBCCES).
To become certified as an Autism specialist
- Have either a Master’s Degree & 2 years of experience in the field or a Bachelor’s degree & 10 years of experience working with autism
- Pay the required registry free
- Have completed 14 autism-related CE hours
- Pass the online Autism Competency Exam
- Pay Registry Fee

Brain Injury (CBIS ): An occupational therapist specializing in brain injury ( also called a Certified Brain Injury Specialist) helps patients who have experienced traumatic and non-traumatic brain injury. OTs who specialize in brain injuries can help those with traumatic brain injuries caused by traffic accidents and falls. They can also help those with non-traumatic injuries, such as those from tumors and Alzheimer’s disease. This type of OT helps patients plan their routine, return to work, return to hobbies, keep social dates, sleep hygiene, motivation and planning strategies, emotion regulation and cope with fatigue.
- 500 hours of currently verifiable direct contact experience with an individual or individuals with brain injury (through paid employment or academic internship; volunteer work does not count)
- Applicants must have a high school diploma or equivalent
- The class currently costs $325 and is provided by a CBIST (Certified Brain Injury Specialist Trainer) through the Brain Injury Association of America

Complex Environmental Modification OT (CEM): CEM’s are alterations, modifications, or creations of new spaces to meet the needs of an individual, family, group, or community to preserve or facilitate optimal participation in daily life. This type of therapist will look around your home, school, or workplace to see if any modifications can be made to make a person’s life easier. (ramps, wider doors, support bars in restrooms, lower or higher cabinets, rug removal, construction changes needed, etc).
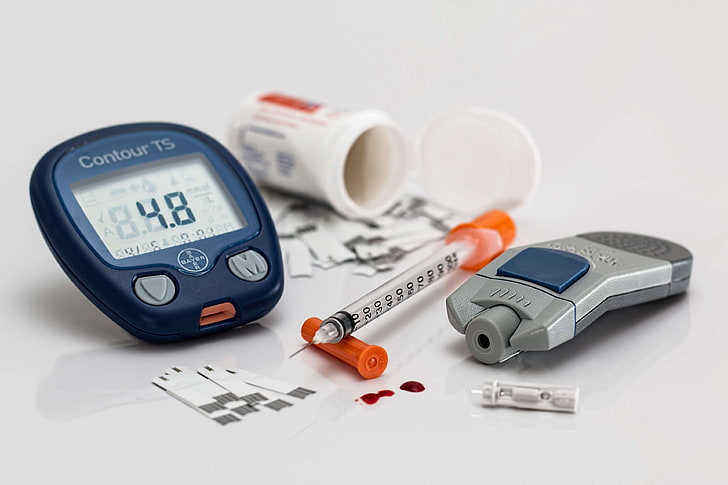
Diabetes: This type of occupational therapy helps those with diabetes learn about and manage their disease.
Many patients with diabetes experience a shift as they get older. They transition from their parents managing their diabetes to managing it by themselves. Occupational therapy has shown to have positive results for those who struggle with maintaining glucose levels and need help with self-managing their diabetes.
An OT can help a patient with things like:
- Diabetes education
- Glucose monitoring
- Diet
- Medication management
- Physical activity assessment
You can pursue your Certified Diabetes Care and Education Specialist (CDCES) credential through the Certification Board for Diabetes Educators (CBDE). Eligible candidates have a current occupational therapist license, at least two years of experience and at least 1,000 hours providing diabetes-related care.

Driving and Community Mobility: As an occupational therapist, you can pursue your Certified Driver Rehabilitation Specialist (CDRS)® credential from the Association for Driver Rehabilitation Specialists. To earn the certification, you pass a certification exam and agree to a code of ethics. You can maintain the CDRS by completing at least 30 hours of continuing education every three years. These are some ways OTs who specialize in driving rehabilitation can help their patients:
- Selecting the best adaptive equipment
- Teaching drivers about defensive and safe driving
- Showing drivers how to use adaptive equipment
- Allowing people to be independent when driving
To become an occupational therapist with this training, you must:
- Be a healthcare practitioner (including OT) with 832 hours of direct, hands-on experience providing driver rehabilitation services
- Completion of a formal certification exam
- Attestation to adhering to ADED’s code of ethics
- Maintain 30 hours of required continuing education every three years

Feeding, Eating, and Swallowing (also called dysphagia) – These are considered activities of daily living (ADL’s) and enable basic survival and wellbeing. Occupation-centered intervention focuses on the components that enhance a person’s ability to participate in eating and feeding ADL’s. Therapists include the family and others involved with the client in in the intervention process. Interventions can include environmental modifications, positioning, use of adaptive equipment, eating and swallowing strategies, remediation techniques, and client and caregiver education.
Dysphagia is a medical term for difficulty swallowing any liquid (even saliva) or solid material. Over time dysphagia can cause dehydration, chest infections, and weight loss.
While similar sounding to the word “Dysphasia” – they have a slightly different spelling and different meanings. Dysphasia is defined as speech disorders in which there is impairment of the power to expression by speech, writing, or signs or impairment of the power of comprehension of spoken or written language.
Dysphagia (difficulty swallowing) can be a painful condition. In some cases, swallowing is impossible. It is classified into 4 different categories: oropharyngeal, esophageal, esophagogastric, and paraesophageal.
Signs of dysphagia include:
- coughing or choking when eating or drinking
- bringing food back up, sometimes through the nose
- a feeling that food is stuck in throat or chest
- a gurgly, wet-sounding voice when eating or drinking
- drooling and problems chewing food
To pursue this certification as an Occupational Therapist, you must:
- Complete the SOS Approach to Feeding 12-week live/interactive online course
- Complete the written exam at the end of the course

Geriatric OT: Geriatric occupational therapists usually work with a team of medical professionals to help aging patients continue living as independently as possible. They work with the elderly to teach them exercise and rehabilitation techniques that make completing daily tasks much easier. They help older people resolve physical difficulties by encouraging them to return home and live their daily lives longer in their own homes. They help by working with them to prevent falls, teach self-care skills (such as cooking, sleeping, dressing, and grooming), achieve a safer, more accessible home (wheelchair ramps, etc), use equipment that can assist with mobility and everyday living (shower rails, transfer chairs, wheelchairs, shower seats, etc). These and other tasks can become harder or painful for an older adult to do on their own due to an injury or health condition, disability, or in some cases because of normal aging.
An OT can also help with more complex daily activities (instrumental activities of daily living). These tasks require more thinking (cognitive) or social skills, and include:
- Food shopping and making meals
- Using a phone or computer
- Cleaning and doing laundry
- Managing daily medicines
- Managing finances
- Driving
There is an unprecedented need for patient, skilled, and caring occupational therapists specialized in geriatric care to help evaluate and treat the injuries and illnesses associated with aging. If this interests you, check your eligibility to acquire this training.
- Minimum of 3 years practicing as an OT (two years if you completed an AOTA-approved Fellowship Program)
- Minimum of 3,000 hours in any capacity of gerontology within the past 5 years – may include may include direct intervention, supervision, teaching, consultation, administration, case or care management, community programming, or research
- Minimum of 500 hours delivering OT services in gerontology or certification area within the past 5 years
- Provide Verification – providing proof can be acquired through many ways.
- Provide Attestation – Applicants to the Advanced Certification Program will be required to attest that the information provided in the application is true and complete to the best of the applicant’s knowledge, and that the applicant is in compliance with the Occupational Therapy Code of Ethics.
OTs sometimes work with occupational therapy assistants and aides (OTAs), who can also help with treatment.

Hand Therapy: A hand therapist is trained in kinesiology, physiology, and anatomy. Hand therapy is a component of occupational therapy (OT) or physical therapy (PT), either helping individuals complete everyday tasks with their impairment or working on the impairment directly by improving mobility and lessening pain. A hand therapist, through advanced study and experience, specializes in treating individuals with conditions affecting the hands and upper extremity ( including the hand, wrist, elbow, and shoulder). A qualified hand therapist can evaluate and treat any problem related to the upper extremity. They provide post-operative rehabilitation, preventative, non-operative or conservative treatment, or industry consultation. They work closely with physicians and patients to provide a continuum of care, starting within days of injury or surgery and continuing until the patients return to work and have a productive lifestyle.
Occupational hand therapy involves helping patients use writing utensils, silverware, a toothbrush, and other common handheld items. Whereas PT focuses on reducing pain and increasing mobility, OT focuses on improving fine motor skills, visual-perceptual skills, and cognitive skills.
Hand therapists can treat the following:
- Amputations
- Arthritis and rheumatic diseases
- Burns
- Carpal tunnel or cubital tunnel syndrome
- Crush injuries
- Cysts and tumors
- Dislocations
- Dupuytren’s disease (one or more fingers become bent)
- Fine motor skill deficiencies
- Fractures
- Ganglion Cyst
- Golfer’s Elbow
- Hand Pain
- Repetitive Motion Disorder (or De Quervain’s tenosynovitis)
- Tendonitis
- Tendon injuries
- Tennis Elbow
- Trigger Finger
- Sprains/strains
Hand pain can be disruptive to your daily activities, and it’s crucial to address your pain issues to be appropriately diagnosed, treated, and managed as soon as possible.
To get certified as a hand therapist, you must:
- Work as an occupational therapist or physical therapist for three years
- 4,000 hours of direct hand therapy practice experience (obtained in any country). Upcoming and projected hours are not accepted prior to the application deadline.
- Must pass the Certified Hand Therapist exam
- Renew credential every five years through continued education and participation in hand and upper extremity therapy.
You can find more information about becoming a certified hand therapist from the Hand Therapy Certification Commission.

Hippotherapy: The term hippotherapy refers to how occupational therapy, physical therapy and speech-language pathology professionals use evidence-based practice and clinical reasoning in the purposeful manipulation of equine movement as a therapy tool to engage sensory, neuromotor and cognitive systems to promote functional outcomes. Hippotherapy is a type of therapy in which a therapist uses the characteristic movements of a horse to provide carefully graded motor and sensory input. Unlike therapeutic horseback riding (where specific riding skills are taught), the movement of the horse is a means to a treatment goal when utilizing hippotherapy as a treatment strategy.
Hippotherapy has been used to treat patients with neurological or other disabilities, such as autism, cerebral palsy, arthritis, multiple sclerosis, head injury, stroke, spinal cord injury, behavioral disorders and psychiatric disorders.
There is no such thing as “hippotherapy service” nor are there “hippotherapy programs”. Therapists do not “perform hippotherapy”. Licensed therapy professionals in PT, OT and SLP incorporate equine movement into their plans of care for their patients as a ” therapy tool”. Please refer to the description of hippotherapy on the AHA website.
Incorporating equine movement as a therapy tool is regarded as use of a standard practice tool/strategy by APTA, AOTA and ASHA — Hippotherapy must not be treated as separate service from PT, OT or ST services. Even in casual conversation, it is important to describe it accurately.
See American Hippotherapy Association or Hippotherapy Certification Board for more information about this type of therapy.


Hydrotherapy (also called aquatic therapy, pool therapy, or balneotherapy): Hydrotherapy is the external or internal use of water in any of its forms (water, ice, steam) for health promotion or treatment of various diseases with various temperatures, pressure, duration, and site. Hydrotherapy has lots of advantages can be a great way to reduce symptoms without medication or other more invasive treatments.
Balneotherapy is the treatment of disease by bathing in mineral springs. Pool therapy is an exercise program that is performed in the water.
Hydrotherapy is an alternative (naturopathic or nonpharmaceutical) treatment, which means it’s not regulated by the U.S. Food and Drug Administration (FDA). There are legitimate benefits that experts have studied that help reduce pain and stiffness.
Hydrotherapy helps with:
- Enhancing balance
- Extending range of motion
- Improving strength
- Maintaining coordination
The warmth of the water allows your muscles to relax, eases the pain in joints. The buoyancy of the water helps take pressure off of joints by reducing the force of gravity that is compressing the joints, and assists with progression of exercise. The water helps to relieve pain, improve muscle strength, and increase the range of movement in your joints.
You can get your aquatic therapeutic exercise certification (ATRIC) from the Aquatic Exercise Association after passing a 100-question exam.

Kinesio Taping (also known as kinesiology or elastic therapeutic tape): Kinesio Taping is a technique designed to work with the body’s natural healing process while providing rehabilitative support and stability to muscles and joints. It can be used to decrease pain, reduce inflammation, and relax overused or tired muscles. Kinesio Taping Method is a therapeutic tool utilized by rehabilitation specialists in all programs (pediatric, geriatric, orthopedic, neurological, oncology and others) and levels of care (acute care, inpatient rehabilitation, outpatient, home care and Day Rehab).
The idea of using elastic tape to mimic the therapist’s hands was first presented by a Japanese Chiropractor named Dr Kenzo Kase in the 1970s who wanted to develop a supportive and stabilizing tape that acted as human skin. Ever since, his invention has been used as a preventative and restorative treatment. Since then, it became the modality used in pain management, soft tissue injury, tissues and joints malalignment, edema, and more.
General contraindications are:
- Malignancy
- Infection, cellulitis
- Open wound
- DVT
- Previous allergic reaction to Kinesio Tex Tape
General precautions are:
- Diabetes
- Congestive heart failure (CHF)
- Patient receiving dialysis/Kidney disease
- Organ transplants
- Pregnancy
Kinesio (Ka knee see o) tape is a flexible tape that supports and stabilizes joints, muscles, and ligaments as they bend, contract, and extend. You may have seen athletes at sporting events wearing long strips of brightly colored tape strategically placed on or near their joints. The tape is typically made of cotton and spandex with a heat-activated acrylic adhesive to keep it in place on the skin.
Currently, 4 types of tapes are available for Kinesio Taping Method applications for humans (Tex Classic, Performance, Gold, Gold Light Touch Plus) and 2 types for animals (Kinesio Equine and Kinesio Canine). Each clinician can choose the most appropriate type of tape based on the desired outcome and the client’s skin condition. When an untrained individual considers taping, it is suggested to use Classic or Performance+ Tape.
The following are tape types and their characteristic:
- Kinesio Tex Classic: the original tape that received several upgrades over time, the most universal as it can be used for all applications and ideally on healthy skin.
- Kinesio Tex Performance+: different, looser pattern on the tread, polyester, and cotton blend best for sensitive skin when higher tensions on the tape are desired.
- Kinesio Tex Gold: special distribution of adhesive allowing good attachment without requiring large surface area, good for low tension applications and available only for trained professionals.
- Kinesio Tex Gold Light Touch Plus: adhesive distributed to allow gentle grip, does not last as long as other types. It is used for short-term applications and usually for children and older adults with fragile skin.
- Kinesio Equine: developed to allow the Kinesio Taping method to be used on horses, can be applied directly on horses’ hair, and its taste prevents animals from chewing it.
- Kinesio Canine is used on dogs and works well with dogs’ hair.
It is important to have knowledge of human anatomy to fully understand each advanced level Kinesio Medical Taping application such as Jellyfish, EDF (Epidermis, Dermis and Fascia) Snowflake and Fan Cut Taping to name a few.
The letters CKTP stand for Certified Kinesio Taping Practitioner. In earning and maintaining your CKTP status you are demonstrating your commitment to the highest standards of patient care within the only globally recognized modality for health professionals. Those letters “CKTP” after a name ensure confidence that the practitioner has undergone the necessary training to integrate Kinesio Taping in to their practice.
Go HERE to become certified as a CKTP

Living In Place: Living in Place includes preventive measures for those who wish to remain in their homes indefinitely, along with solutions for special needs to be addressed immediately. The housing and design industry is continuously hit with a high demand for designers to find solutions for individuals with various physical and cognitive needs. While there are similar certifications, only Living in Place addresses uniqueness and teaches the tools that help designers think outside the box to create solutions for each individual client.
Living in place specialists are dedicated to helping individuals age comfortably and safely in their own homes. The first step to becoming a Certified Aging in Place Specialist (CAPS) is to complete a comprehensive training program.
CAPS Program
- Completion of the following courses:
- Marketing and Communicating with the Aging in Place Client (CAPS I)
- Design Concepts for Livable Homes and Aging in Place (CAPS II)
- Details and Solutions for Livable Homes and Aging in Place (CAPS III)
- Completion of online CAPS graduation application
- Signed copy of CAPS code of ethics pledge
- Submit application fee
Another training program is:
Living In Place Institute
The Living in Place Institute creates a worldwide network of professionals through professional education and awareness programs, as a fundamental shift to a simple, complete approach of improving home Accessibility, Health and Safety, creating beautiful, functional and connected environments that improves lives and promotes independence and dignity, for all ages and abilities.
The primary education courses include:
- Certified Living In Place Professional (CLIPP)
- Home & Accessibility Trade Specialist (HATS)
Low Vision – Low Vision is the term used to describe significant visual impairment that cannot be corrected fully with glasses, contact lenses, medication or eye surgery. Low vision is a general term that refers to a permanent functional vision loss
Low vision occupational therapists focus on reducing the impact of a patient’s vision impairment on their daily routine and helping them live an independent life. Low vision occupational therapists achieve this by teaching their patients new skills, modifying their tasks or making changes to their environments, and at times, collaborating with vision experts such as optometrists, ophthalmologists and teachers of the visually impaired. They provide environmental adaptations and advice on lighting, managing glare, enhancing contrast and improving home safety. They teach strategies to maximize use of residual or remaining vision.
Occupational therapy for individuals with low vision can benefit those with:
- Macular Degeneration
- Glaucoma
- Diabetic Retinopathy
- Visual field loss caused by neurological insult (ex., stroke, head injury)
- Retinitis Pigmentosa
- Other difficulties associated with low vision
The rehabilitation plan may include magnification, enhanced contrast, task lighting, colored filters, computer/cell phone adaptations and even text to speech options.
The Certified Low Vision Therapist (CLVT®) certification is offered by the ACVREP. They also offer certifications in vision rehabilitation therapy and assistive technology. Also available through CLVT Certification.
- Have at least a Bachelor’s degree in Occupational Therapy
- Successful completion of 350 hours of low vision experience under an MD or OD practicing in low vision
- Pass the certification examination

Lymphedema – Lymphedema cannot be cured, only managed. The goal of treatment is to reduce the swelling or keep it from getting worse, and to relieve symptoms.
Lymphedema is defined by the National Lymphedema Network as “an abnormal collection of lymphatic fluid in the tissues just beneath the skin. Lymphedema develops when a body region, where lymphatic vessels and lymph nodes are missing or impaired, becomes overloaded with lymphatic fluid. Typically, this will be seen in the arm or leg but we also see it in other body areas such as the head and neck, chest, and trunk”.
In the early stages of lymphedema, mild swelling can often be conservatively managed with manual lymphatic drainage (MLD), compression garments, exercise, and elevation of the affected limb to encourage lymph flow. More severe or chronic swelling typically requires the addition of compression bandaging to reduce swelling prior to being fitted with compression garments.
Occupational therapy services are indicated to assist clients to concurrently address integration of lymphedema self-management techniques into daily living and any occupational performance complaints associated with lymphedema onset. Occupational therapists can enhance their professional practice by pursuing continuing education opportunities to develop specialized clinical skills in lymphedema assessment and treatment.
Management is a 4-part system best completed with a CDT.
- Skin Care
- Exercise
- Manual Lymphatic drainage (clinic and home based): This is a hands-on technique to help with the flow of the fluid. Lymphatic massage will not be complete without the other 3 parts. If this is the goal, a massage therapist who specializes in lymphedema should be contacted.
- Compression
- Phase 1 or Reduction: The goal of this phase is to get you smaller. Short-stretch bandage wrapping (not an ace wrap) and Velcro wraps are options at this stage. Phase 1 lasts as long as the size of the area is going down and you are able to tolerate the wrapping.
- Phase 2 or Containment: The goal of this phase is to keep you at your current size. A compression sleeve/stocking (lasts 6-7 months) is used or a Velcro wrap may be continued. A glove or gauntlet is often used with a sleeve.
Working with a Certified Lymphedema Therapist (CLT) is a key component of treatment interventions for clients with lymphedema.
Lymphedema can be treated with:
Exercise. Moving your swollen arm or leg may help the lymph fluid to drain, thus reducing the swelling.
A compression sleeve or stocking. This garment fits tightly on your swollen arm or leg, helping the lymph fluid flow out.
Massage therapy. A special kind of massage called manual lymph drainage can help push the lymph fluid out of the swollen part of your body.
A pneumatic pump. A machine inflates a sleeve that you place on your swollen arm or leg, helping lymph fluid flow out.
Weight loss. In patients who are overweight, lymphedema related to breast cancer may improve with weight loss.
Surgery. If lymphedema is severe, a doctor may suggest that you get an operation. Several options are available.
To become an Occupational Therapist who acquires a certification as a Certified Lymphedema Specialist (CLT), you must:
- Be a licensed occupational therapist with a current, unrestricted licensure as an RN, OT, COTA, PT, PTA, MD, DO, ATC, DC or Massage Therapists who have completed 500 massage school hours and/or National Therapeutic Massage and Bodywork Certification.
- Complete Lymphedema Certification which includes 135 hours of coursework, including 90 hours of practical, face-to-face laboratory instruction. It is taught over 9 consecutive days. It requires 5 working days and 2 weekends to complete.
For more information regarding CLT requirements, see the Academy of Lymphatic Studies for certification locations or the Norton School of Lymphatic Therapy

Mental Health/Psychiatric; or Clinical Anxiety Occupational Therapist: Mental health occupational therapists can work in residential, community and health care center environments. OTs who specialize in mental health can help patients in areas such as:
- Cognitive assessment
- Socio-emotional skills
- Sensory strategies
- Group process
- Therapeutic alliances
OTs may focus on aspects of life including nutrition, independent living, job readiness, life skills and money management. Mental health OTs help patients learn to be independent and manage a variety of symptom sets, depending on their mental state or condition. You can receive your board certification in mental health (BCMH) from the American Occupational Therapy Association (AOTA) when you have at least 3,000 hours of experience in the specialty area and at least three years of experience as an occupational therapist.
A Clinical Anxiety Occupational therapist includes utilizing exercises, relaxation techniques, stress management strategies, integrating proper sleep hygiene techniques, biofeedback, creating a more balanced schedule, etc. Occupational therapists can help the client engage in activities and build positive habits. They can also utilize general treatments and recommendations, discuss the client’s strengths, weaknesses, and encourage them to participate in meaningful activities.
Neurological Occupational Therapist (also called Neuro or Neurorehab): Neuro OTs work with individuals who have sustained life-changing injuries. They have experience working with people that have a broad range of conditions that fall under two distinct headings; acquired brain injury and progressive conditions. A Neurorehab program with Neurorehap therapists can be found in a variety of settings that include acute care, rehabilitation centers, home and outpatient.
The aim of an occupational therapist is to enable clients to manage their day to day tasks and activities in a way that contributes to their physical, social and emotional well-being. An OT can help if a person is having difficulty performing daily routines, if there are concerns about balance/safety, vision, memory, or cognition.
The occupational therapist will work with the client to address dysfunction using interventions that may look at altering the way a task is performed, adapting the physical environment, teaching the person a new skill or working with them to regain old ones. The occupational therapist works closely with an interdisciplinary team of physicians, physical therapists, speech therapists and audiologists to achieve the best possible outcomes for our patients.
- Completion of at least one of the following courses (can be completed in two weeks (or over a series of weekends):
- Course in the Management of Adults with Stroke and Brain Injury
- NDT/Bobath Certificate Course in the Management & Treatment of Children with Cerebral Palsy and Other Neuromotor Disorders certification course
- Hold an active NDTA membership.
Apply for the certification within 12 months of successful course completion (with a $150 application fee if submitted after 30 days of the course end date).
You can also get your Certified Neuro specialist (CNS), CNS Advanced, or Certified Neuro Practitioner through The Neuro Specialist Institute.

Pediatric OT: This specialization is best for occupational therapists who enjoy working with children, can explain complex ideas simply and know how to be fun and playful during a visit. A pediatric occupational therapist works with children to develop the skills they use every day, in the areas of cognitive skills, motor skills, social development and establishing self-care. This includes activities such as:
- Grooming
- Dressing
- Using utensils
- Writing and coloring
- Play activities
This type of OT assesses the needs of the child and determines any delays or potential limitations. They then work with the child to enhance their skills. The goal is to help them become self-sufficient adults.
(ADHD, Developmental disorders, poor vison or hearing, school trouble, learning disabilities)
Requirements for Certification in Pediatrics:
- Professional degree in OT
- Certified or licensed by and in good standing with an AOTA-recognized credentialing or regulatory body
- Minimum of 3 years practicing as an OT
- Minimum of 3,000 hours in any capacity of pediatrics
- Minimum of 500 hours delivering OT services in pediatrics within the past 5 years

Physical OT: An occupational therapist designs and implements physical rehabilitation interventions that are client-centered, contextually relevant, and evidence-based to facilitate optimal occupational engagement seeking Board certification in physical rehabilitation must meet the following requirements.
When looking for be Board certified in Physical Rehabilitation check out the American Occupational Therapy Association.
Eligibility includes:
- Professional degree in OT
- Certified or licensed by and in good standing with an AOTA-recognized credentialing or regulatory body
- Minimum of 3 years practicing as an OT
- Minimum of 3,000 hours in any capacity of physical rehabilitation
- Minimum of 500 hours delivering OT services in physical rehabilitation within the past 5 years
- Verification of employment
- Passing of the Board Certification Physical Rehab exam (starting July 2023)

Saebo: Saebo is a business that creates upper limb rehabilitation equipment. Those who become Saebo Certified Therapists are knowledgeable in this equipment and how it’s used to help patients suffering from neurological disorders, such as a stroke.
Occupational Therapists who want to be certified, must:
- Licensed occupational or physical therapist or COTA/PTA
- Have experience with fabricating and fitting splints/orthotics
- Have experience with evaluation and treatment of neurological patients
- Currently have an active caseload consisting of neurological patients that are appropriate for the Saebo program

School System: School-based occupational therapy practitioners are occupational therapists (OTs) and occupational therapy assistants (OTAs) who use meaningful activities (occupations) to help children and youth participate in what they need and/or want to do in order to promote physical and mental health and well-being. Occupational therapy addresses the physical, cognitive, psychosocial and sensory components of performance. In schools, occupational therapy practitioners focus on academics, play and leisure, social participation, self-care skills (ADLs or Activities of Daily Living), and transition/ work skills. Occupational therapy’s expertise includes activity and environmental analysis and modification with a goal of reducing the barriers to participation.
School setting occupational therapists focus on helping students succeed in their school environment. This position requires experience and knowledge about lifespan and conditions, evaluation, intervention, and systems, laws, and service delivery systems relevant to the school system client. School-based OTs must address deficits that have an educational impact. This is opposed to a medical model in which occupational therapy services can address any deficit area for the sake of remediating a deficit (as long as funding sources allow). While these often may end up being the same deficits, the difference is that in the school system, those deficits have to be impacting a student’s access to their education.
Those wanting to work in the school system must have a degree in OT and apply for AOTA’s Specialty Certification in School System (SCSS, SCSS-A) through the AOTA.
As part of an application, you must be able to show that you’ve been practicing as an OT for a minimum of 5 years and that you’re licensed by and in good standing with an AOTA-recognized regulatory body. Contact AOTA for a list of all required application materials.

Seating and Mobility Specialist (SMS): The Seating and Mobility Specialist (SMS) is a specialty certification for professionals working in seating and mobility. A certified Assistive Technology Professionals (ATP) and Seating and Mobility Specialists (SMS) evaluates the client in their home environment, determines the client’s mobility needs based on their medical history, current physical and cognitive presentation and medical necessity; provides assistive technology and advice for those needing seating, positioning, or mobility who have disabilities.
The primary goal of an occupational therapist with this specialty is to be an advocate for their clients and to help maintain their current level of independence as it pertains to performing Mobility Activities, and Instrumental Activities of Daily Living (ADL/IADL).
Some of the services provided include:
- Thorough consultation and evaluation with the client and team members to determine seating and mobility needs.
- working with different types of fittings, and follow-up for both manual and power wheel chairs, seating systems, standers, adaptive car seats, adapted chairs, and adaptive bath equipment.
- Recommend and promote of integration of other assistive technology.
- Interaction with the referral source, school personnel, employers, primary therapists, physicians and others to assure quality of care.
- Follow-ups scheduled to assure fit, use and prompt repair of equipment.
The SMS exam is focused specifically on seating, positioning, and mobility. Those occupational therapists interested in this certification should look at the Rehabilitation Engineering and Assistive Technology Society of North America (RESNA), and review the requirements:
- ATP certification
- 1,000 hours or more in seating and mobility-related service with consumers at any time in your professional experience
- Two types of professional activities completed in the last 5 years: Continuing education, client service delivery, advocacy, mentoring, presentation, publication, leadership

Stroke Rehabilitation: An OT specializing in stroke rehabilitation helps patients recover life skills affected by a stroke. After stroke, occupational therapists work to facilitate and improve motor control and hand function in the stroke-affected upper limb; to maximize the person’s ability to undertake his or her own personal self-care tasks and domestic tasks; to help the patient learn strategies to manage the cognitive, perceptual, and behavioral changes associated with stroke; and to prepare the home and work environment for the patient’s return.
Occupational therapy focuses on providing individuals with the proper skills and tools necessary to achieve their recovery goals. They do so by using a combination of rehabilitation exercises and compensatory tactics. Compensation involves accomplishing a task in a different way than before, whereas rehabilitation involves accomplishing a task in the same way as before the stroke.
Occupational therapists focus on addressing any areas that impede the survivor’s ability to accomplish activities necessary to fulfill their daily roles. This involves actively collaborating with the survivor to find out what activities are most important to them to establish therapy goals.
This may include:
- Assessing patients, including physical, social and environmental factors
- Motivating patients to partake in regular activities, taking limitations into account
- Providing information on how to make patients’ environment safer
- Educating caregivers on suggested changes to the patient’s environment and care to promote independence
- Evaluating driving abilities and making suggestions for safer driving
For more information about occupational therapy after stroke, check out the guide:
There are many certifications a person can pursue to specialize in stroke rehabilitation, including the Certified Neuro Specialist (CNS) credential.
- Licensed occupational or physical therapist
- Complete the educational program, which includes four 8-hour seminars costing a total of $900 for all four courses
- Pass the exam (the current cost of the exam is $150)

Thank you for visiting the HOPE TBI Website.
Please take the time to make a comment, share your thoughts, and tell us what impacted you the most and what brought you here:
https://hopetbi.com/reviews-and-testimonials/
Your input is important to the development and growth of this website, and we like to know what is going on out there in your thoughts.
Thank you for visiting us! We look forward to hearing from you.
